We must trust that everything said to a doctor or a social worker will be held in the strictest confidence. Otherwise, we might not share important information about our health. Maintaining confidentiality in health and social care is crucial. Without it, caregivers can’t develop trusting and lasting relationships with their patients.
If you’re employed in the health and social care sectors, you must know the importance of maintaining confidentiality and keeping people’s information private. To ensure you know your responsibilities, we’ve compiled this short guide on confidentiality in health and social care.
What is Confidentiality in Healthcare?
Confidentiality can be defined as respecting a person’s wishes by keeping sensitive personal information about them from becoming public.
Suppose a patient shares information with a professional like a doctor, nurse, social worker, or support worker – that information must be kept confidential. It can’t be shared with anyone who doesn’t have a professional need to know unless the patient has given their express consent. Confidentiality also applies to any digital records or written notes that have been made.
Why is Confidentiality Important in Health and Social Care?
We all have embarrassing details about our lives that we want to keep to ourselves. You might be fond of an 80s sitcom or have a bad habit of snacking on leftovers in the middle of the night. You might like to spend your free time painting miniatures or reading romance novels. Whatever it is, you probably wouldn’t want that information getting out.
And when it comes to embarrassing information, no one knows more about us than healthcare providers and social care workers. Most likely, you wouldn’t want the details of your last visit to the doctor or a meeting with a social worker to be made public. We must trust health and social care professionals to keep our information private. This expectation of confidentiality in health and social care forms the foundation of the caregiver/patient relationship.
There can be severe consequences for patients if confidentiality is breached. A person may face social stigma if their medical condition becomes known to the community. And if a patient doesn’t trust that their healthcare provider will maintain confidentiality, then they may not provide them with crucial details about their health. Withholding information can lead to a misdiagnosis that results in a person not getting the care they need.
Maintaining confidentiality in health and social care situations is also a legal requirement. By law, healthcare workers have to protect the sensitive personal information of their patients.

How to Maintain Confidentiality in Healthcare
Confidentiality is essential for healthcare workers, but it’s not always clear-cut. There are situations when professionals have to maintain confidentiality. But there are also exceptions where confidentiality rules may have to be waived to protect people’s safety.
Healthcare workers and those in the social care sector must maintain confidentiality about any information relating to:
- A person’s relationships or family
- Details of their health or medical condition
- Personal details such as their name, age, address, banking information and so on
However, in certain circumstances, a professional can break their duty of confidentiality. A professional can only do this if they believe that doing so will protect the patient from harm or protect another person or the general public from harm.
Consent should be obtained from the person in question, if possible. It’s not always possible to obtain consent, however. In some cases, confidentiality must be breached against a person’s wishes.
An example of where a professional may need to break confidentiality is in cases of domestic violence. A social worker may need to inform the police to keep the victim safe. Another example could be where a doctor may need to notify authorities about a patient who has a rare and highly contagious disease. In both cases, consent may be given, or the professional may have to override the person’s wishes.
Sharing a person’s private information with or without their consent is a serious matter. Professionals need to use their judgment and consider each case on its own merits. It’s always a good idea to seek advice from a superior before breaching confidentiality. If you have to share private information about a person, keep records of your actions, inform your superiors, and stay involved to keep the person from harm.
The Five Rules of Confidentiality
Maintaining confidentiality can be difficult. Thankfully, experts at the Health and Social Care Information Centre (HSCIC) compiled a guide for preserving confidentiality in health and social care. In 2013, the HSCIC developed five confidentiality rules, which are still considered best practices today.
The five HSCIC rules about confidentiality in health and social care are:
- Confidential information about service users or patients should be treated confidentially and respectfully.
- Members of a care team should share confidential information when it is needed for the safe and effective care of an individual.
- Information that is shared for the benefit of the community should be anonymised.
- An individual’s right to object to the sharing of confidential information about them should be respected.
- Organisations should put policies, procedures and systems in place to ensure that confidentiality rules are followed.
Important Confidentiality Policy in Health and Social Care
Maintaining confidentiality isn’t just a matter of being a decent person. It’s also the law. And breaking the law has consequences. Below is some primary legislation that applies to keeping people’s information confidential.
The Common Law of Confidentiality
The main principle of the Common Law of Confidentiality is that a person’s details should not be disclosed or used unless the person has given their express consent. Common law confidentiality can, however, be overridden by cases involving a person’s safety, the safety of the public at large or in the public interest.
The Human Rights Act 1998
Article 8 of the Human Rights Act 1998 mandates that people have the right to keep details about their private life, family life, correspondence and homes confidential.
Again, this right can be overridden if the authorities can prove that such an action is required to protect the public or national security, prevent crime or protect the safety of the person in question or others.
The Care Act 2014
The Care Act 2014 provides guidance on situations where caregivers may have to breach confidentiality. The Act states that in cases where privacy is breached, a written report that provides details of the justification must be made and, where possible, the consent of the individual in question should be acquired.
The Data Protection Act 2018 and the GDPR
The Data Protection Act and the GDPR set out how organisations, charities and businesses must collect, store, and process personal data.
The Data Protection Act 2018 and the GDPR mandate that personal data must be:
- Processed in a lawful, transparent and fair manner
- Collected and kept only for legitimate, specified and explicit purposes
- Be accurate and up-to-date
- Limited to what is necessary
- Kept only for as long as necessary
- Processed with appropriate security measures in place
The Health and Social Care (Safety and Quality) Act 2015
The Health and Social Care (Safety and Quality) Act 2015 covers how people in the UK healthcare sector and social care services share patient information with other healthcare professionals. It also guides how patients’ data should be integrated into health and social care systems.
Sharing Information and Managing Confidentiality in Health and Social Care
Health and social care professionals walk a fine line between protecting a person’s privacy and sharing information to support their safety and wellbeing. Good care relies on communication, but only the right information, shared at the right time, with the right people.
This section explores how to share information safely and responsibly while continuing to uphold confidentiality.
Only Share What People Need to Know
Information should only be shared on a strict need-to-know basis. That means only those directly involved in a person’s care, and only if the information is necessary to help that person. For example, a carer might need to know about a person’s allergies, but not their entire medical history.
- Before sharing anything, consider:
- Does this person need the information to carry out their role?
- Is the information directly relevant?
- Can some details be left out?
This applies to conversations, notes, emails, and care records.
Multi-Agency Working and Shared Responsibilities
In many cases, care is delivered by multiple teams or organisations, such as hospitals, social workers and support services. Sharing the right information across these teams is essential to keep people safe. But it must be done securely and with clear boundaries.
Professionals should:
- Use secure, approved communication channels
- Follow information-sharing agreements between organisations
- Always record what has been shared, why, and with whom
It’s also good practice to let the person know who else will be involved in their care and why.
Managing Different Types of Information
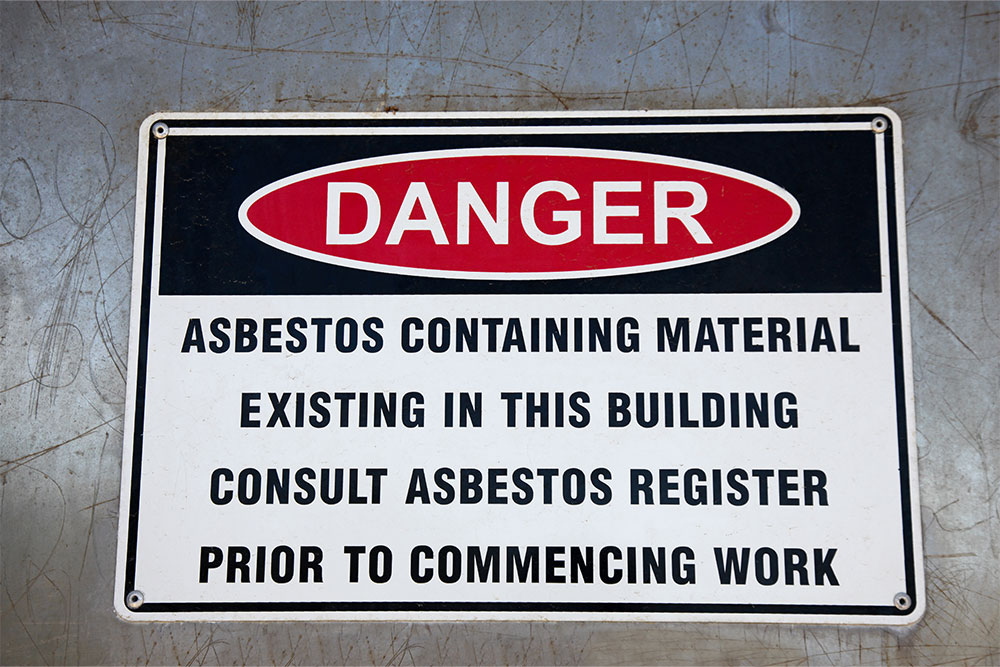
Verbal conversations, written notes and digital records must all be handled carefully:
- Avoid discussing sensitive details in public spaces
- Keep paper records locked away
- Use encrypted systems and secure devices for digital notes and emails
Don’t use personal phones or messaging apps to share care-related information unless your organisation has approved them.
When Consent Isn’t Possible
Whenever possible, get the person’s consent before sharing information. But sometimes, consent can’t be obtained, or a person may say no when sharing is still necessary.
You can share information without consent if:
- There’s a serious risk to the person’s safety or someone else’s
- It’s needed to prevent a crime or serious harm
- It’s required by law or a court order
If you have to share without consent, always:
- Record your decision and the reasons behind it
- Let a manager or the safeguarding lead know
- Share only what’s absolutely necessary
How to Record and Justify Decisions
Every time you share confidential information, keep a clear record. This is important for accountability, legal protection and continuity of care.
Record:
- What you shared
- Who you shared it with
- Why sharing was necessary
- Whether consent was given or not
These notes should be stored securely, just like all other care records.
Cultural Sensitivity in Information Sharing
People from different backgrounds may have different expectations about privacy. Some may want family members involved in every decision. Others may prefer to keep information private, even from loved ones.
It’s important to:
- Respect each person’s preferences
- Avoid assumptions based on culture, religion or background
- Communicate clearly and check understanding before sharing
If in doubt, ask and be led by the person’s choices wherever possible.
Digital Care and Confidentiality
With more care records stored online, there’s a growing need for digital awareness. All staff should:
- Use strong passwords and avoid sharing them
- Lock screens when stepping away
- Report suspicious emails or cyber threats
- Avoid saving personal data to unapproved devices or platforms
Technology makes information sharing easier, but it also increases risk. Staff training and secure systems are vital.
Reflecting on Difficult Decisions
Information sharing can be emotionally challenging. Professionals sometimes face tough calls, especially in safeguarding cases or when someone refuses consent.
Supervision sessions or team meetings are good opportunities to reflect on:
- How the decision was made
- What went well
- What could be improved next time
Sharing responsibility and learning from experience helps everyone make safer decisions in the future.
Online Training for Health and Social Care Professionals
Healthcare and social care workers have serious responsibilities when it comes to confidentiality. Health and safety courses can give you the skills to act in the best interests of your patients.
You can enhance your professional knowledge with our health and safety training courses. All courses are accredited and can be taken online at your convenience.